What is COPD?
COPD, or chronic obstructive pulmonary disease, is a chronic inflammatory lung disease that reduces the amount of air that flows in and out of the lungs, making it difficult to breathe.
COPD includes 2 main conditions: chronic bronchitis and emphysema.
Most people who have COPD have both chronic bronchitis and emphysema, but the severity of each varies from person to person.
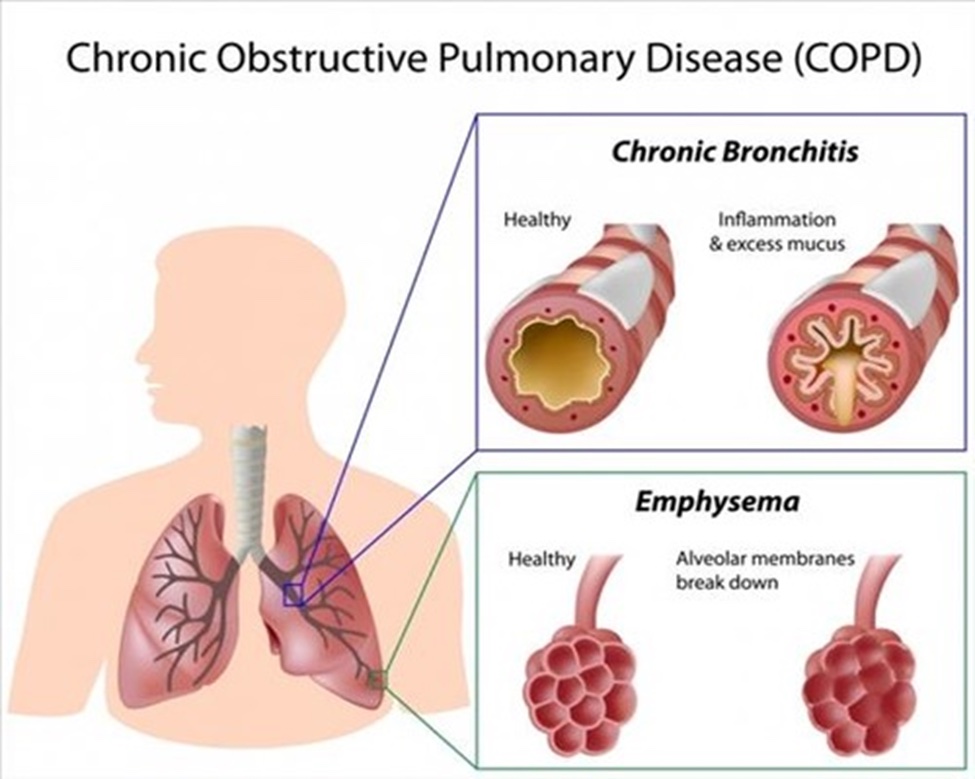
Chronic Bronchitis – is caused by repeated or constant irritation and inflammation in the lining of the airways. With chronic bronchitis, the lungs produce more mucus than normal, which can block the airways. This makes it difficult to get air in and out and causes shortness of breath.
Emphysema – causes damage to the walls between the air sacs in the lungs, causing them to lose their elasticity. Normally, these sacs are elastic or stretchy. When you breathe in, each air sac fills up with air, like a small balloon. When you breathe out, the air sacs deflate, and the air goes out. With emphysema, the airways collapse when you exhale, trapping air in your lungs – which causes shortness of breath. Over time, the air sacs lose their shape, which also allows less oxygen to enter the bloodstream and body.
Causes & Risk Factors
COPD can often be prevented, mainly by not smoking. However, up to 30% of people with COPD have never smoked. Causes of COPD include:
- Smoking. Cigarette smoking is the leading cause of COPD. Most people who have COPD smoke or used to smoke. The more years you have smoked and the more packs you have smoked per day, the greater the risk. Pipe smokers, cigar smokers and marijuana smokers may also be at risk, as well as those who have been exposed to large amounts of secondhand smoke.
- Childhood asthma. Asthma is a chronic inflammatory airway disease and is believed to be a risk factor for developing COPD. The combination of asthma and smoking increases the risk of developing COPD.
- Occupational exposures. Long-term exposure to chemical fumes, vapors and dust in the workplace can cause chronic irritation and inflammation in the lungs and increase the risk of developing COPD.
- Exposure to fumes from burning fuel. Those in developing countries, who are exposed to fumes from burning fuel for cooking and heating - in poorly ventilated homes - are at increased risk of developing COPD.
- Genetics. A rare genetic condition called alpha-1 antitrypsin (AAT) deficiency, which can cause COPD at a young age. AAT deficiency is an inherited disorder that can lead to COPD. Alpha-1 antitrypsin is an enzyme that helps protect your lungs from the damaging effects of inflammation. With AAT deficiency, the body does not produce enough alpha-1 antitrypsin, increasing the likelihood of lung damage from exposure to irritants such as smoke, chemicals, and dust. Global Initiative for Chronic Obstructive Lung Disease (GOLD) Guidelines recommend that everyone diagnosed with COPD be tested for AAT deficiency (with a blood test) to determine if their COPD is from alpha-1 antitrypsin deficiency.
Symptoms
Symptoms of COPD typically develop at mid-life. In the beginning, many people experience only mild symptoms or have no symptoms at all. As the disease progresses, more symptoms occur. Common symptoms include:
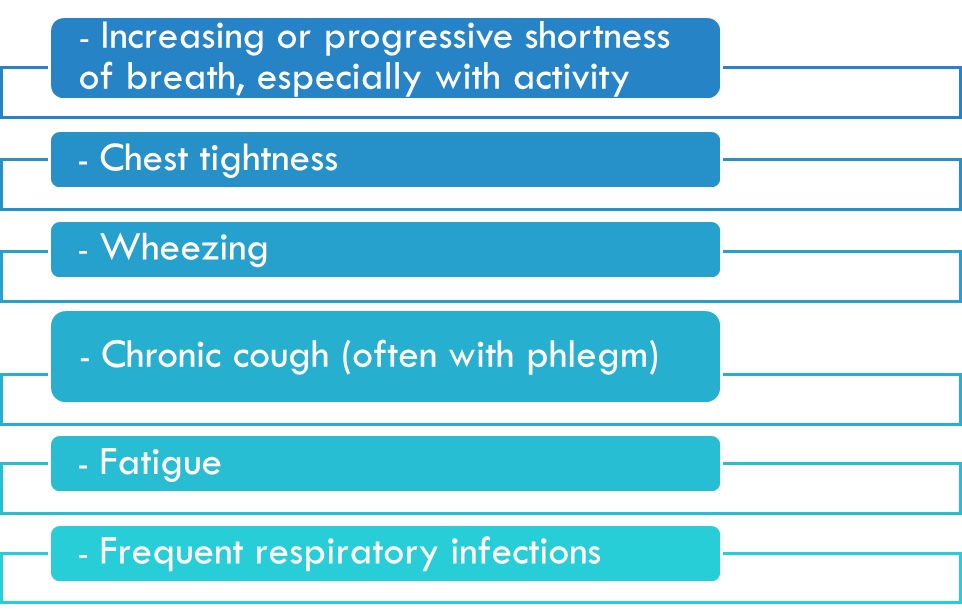
This list is not inclusive; symptoms vary from person to person. In some cases, COPD also causes:
As COPD progresses, many people find it more difficult to perform their normal daily activities. During flare-ups, or exacerbations, symptoms often become worse and require extra treatment at home or admission to the hospital. Severe flare-ups can be life threatening. Many people with COPD have other medical conditions such as heart disease, osteoporosis, musculoskeletal disorders, lung cancer, depression, and anxiety.
Diagnosis & Staging
If COPD is suspected, your doctor will perform a detailed review of your symptoms and medical history, to include:
- Risk factors, such as smoking and occupational or environmental exposures
- History of respiratory illnesses/symptoms
- Medical history, including asthma, tuberculosis, HIV and other respiratory and non-respiratory diseases
- History of comorbidities that may limit or restrict activity, such as osteoporosis, musculoskeletal disorders, anxiety and depression
Spirometry is necessary to confirm and stage COPD. Additional diagnostic tests may also be ordered and can be seen below:
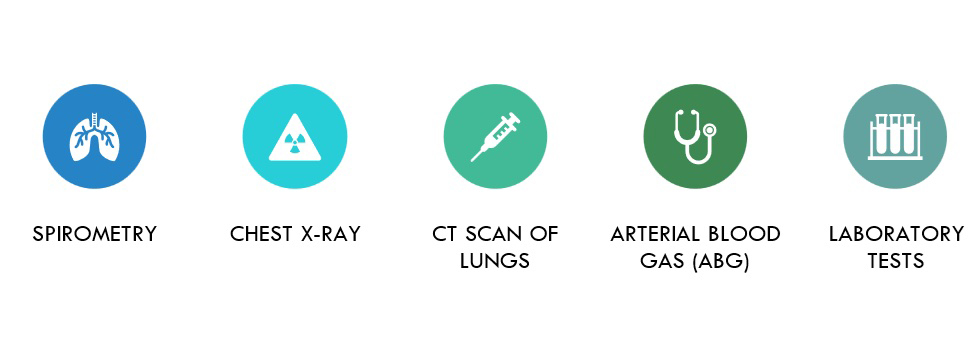
Spirometry is a type of pulmonary function test, or PFT. During spirometry, you will blow into a tube that is connected to a machine that measures how much air your lungs can hold and how much air you can forcefully blow out.
During the test, you may be given a bronchodilator (Albuterol) to see if there is any change in your lung function after the treatment.

Based upon the results of the spirometry testing, COPD will be confirmed or ruled out. If the test confirms COPD, your doctor will also be able to tell you what stage of COPD you have. Staging is used to identify the severity of COPD and will help your doctor determine the best treatment plan for you. The Global Initiative for Chronic Obstructive Lung Disease (GOLD) staging system is widely used and will grade the severity of COPD based upon:
- Spirometry or Pulmonary Function Test (PFT) results
- Severity and type of symptoms
- The number of moderate to severe flare-ups you’ve had in the past year
Stages of COPD
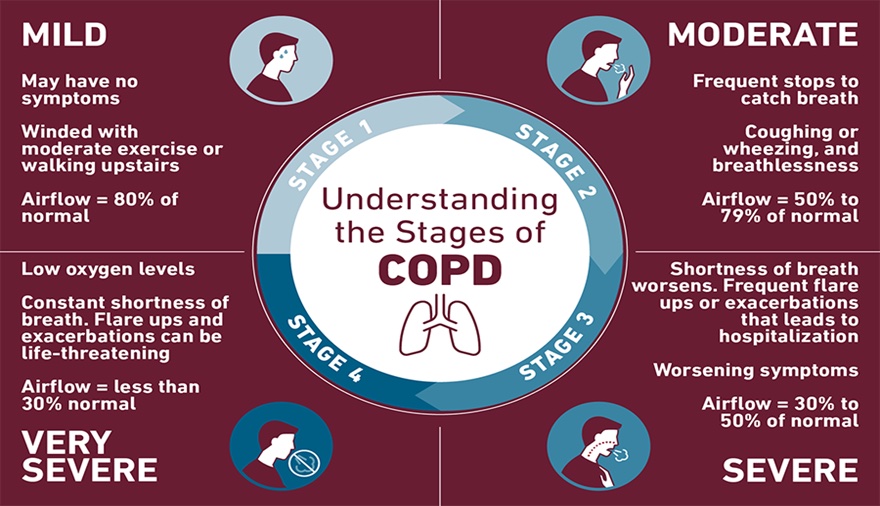
Source: Templehealth.org (2020)
Living with COPD
While there is no cure for COPD, early diagnosis and treatment are important to help slow the progression of symptoms and reduce the risk of flare-ups, or exacerbations.
There are actions that can be taken to help improve overall health and control COPD:
- Stop smoking
- Exercise regularly
- See your doctor regularly
- Maintain a healthy weight
- Follow the COPD Action Plan
- Get vaccinated against pneumonia, influenza and coronavirus. Other vaccinations may be necessary. If you are unsure about your vaccination history, or which vaccines are right for you, talk to your doctor.
When properly managed, many people with COPD are able to control their symptoms and improve their quality of life, in addition to reducing their risk of other related conditions. An important element in the self-management of COPD is the COPD Action Plan. The COPD Action Plan is a tool that should be used daily to assess your respiratory status. This is important for early recognition and intervention, in case of an exacerbation or flare up. Oftentimes, people with chronic lung disease have signs and symptoms of a lung infection or inflammation for several days or weeks before seeking treatment or notifying their provider. This window is a period of time where these signs and symptoms could have been addressed and prevented the exacerbation from progressing. In some situations, delaying care for a COPD exacerbation can result in an emergency department visit, hospitalization or even death. The good news is that there are often red-flags of a flare; recognizing these signs and symptoms is key - which is why the COPD Self-Management Action Plan is such an important tool for people living with COPD.
COPD Action Plan
The COPD Self-Management Action Plan, which can be seen below, has three zones: Green, Yellow, and Red. The left column lists the signs and symptoms for each zone and the right column lists the appropriate actions for each zone. It is important to note that the list of signs and symptoms is not comprehensive; you may experience additional symptoms. The COPD Action Plan should be completed with your physician or healthcare provider. He or she will recommend actions for you to take in each of the zones, based upon your specific healthcare needs, by checking the appropriate boxes.
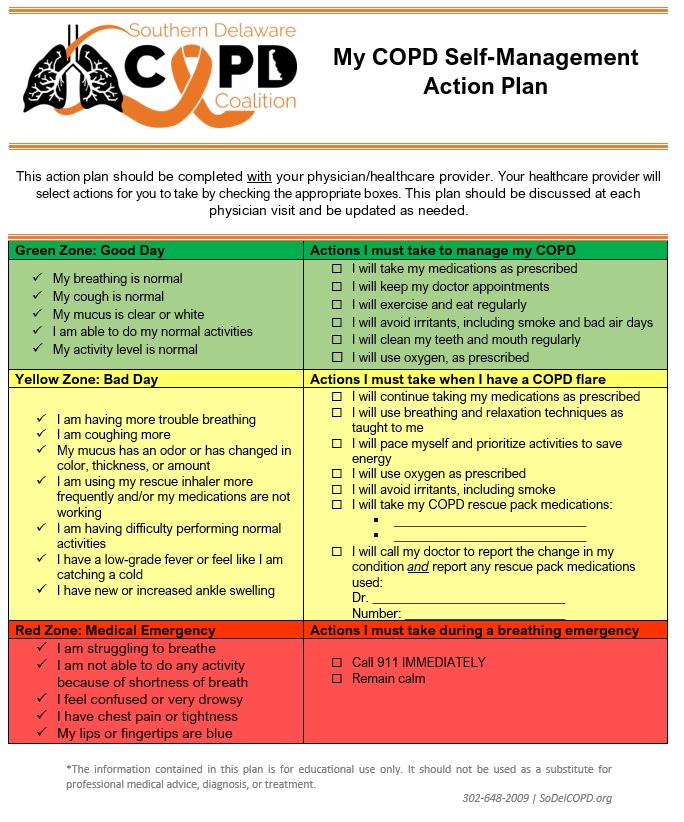
It is important to assess your symptoms daily and to recognize how you feel on a good day, or when you are in the Green Zone. Recognizing this will help you should you start to experience symptoms of the yellow zone. While it is normal for the symptoms of COPD to fluctuate from day to day, if your symptoms persist for more than two days and/or worsen, this is an exacerbation or flare. If you’re having any of the signs or symptoms of a COPD exacerbation, don't wait for your next appointment to call your provider. Follow the action for the Yellow Zone to get the necessary treatment for any lung inflammation or infection. Don't wait for symptoms to become so severe that you experience a medical emergency, or the Red Zone. Again, if you notice your symptoms early and contact your healthcare provider, your provider may be able to change or add medications that will make you feel better, and prevent you from progressing to the Red Zone. Please note that you should never stop or change medications without discussing with your healthcare provider. It is also important to note that signs and symptoms may be the same or different from one flare-up to another. Use your Action Plan to monitor your symptoms daily.
If you have any questions about your COPD Self-Management Action Plan, please feel free to contact us @ info@sodelcopd.org.
